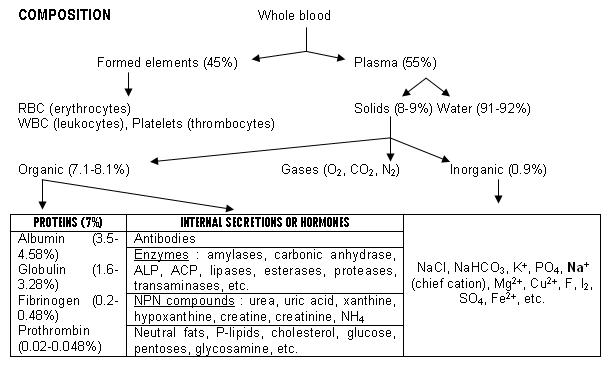
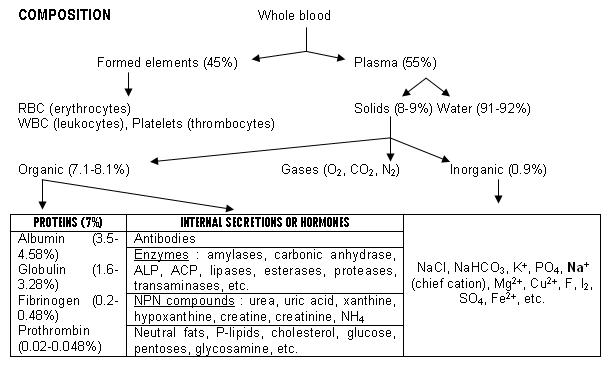
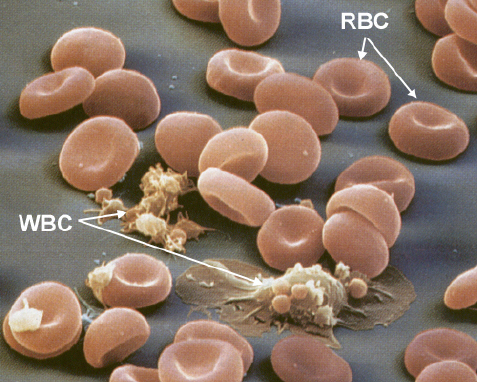
BLOOD, the fluid connective tissue of the human body, consists of liquid matrix called plasma, in which formed elements such as RBC, WBC & platelets remain suspended.
FUNCTIONS
Along with lymph & tissue fluids, blood serves as the connective link between the individual cells of distant organs & tissues. The other functions are:-
A. TRANSPORT
2. RESPIRATORY GASES: O2 from lungs to tissues & CO2 back to lungs from tissues.
3. HORMONES: Endocrine hormones are carried to distant target glands only through blood. Eg: ACTH, GnRH, etc.
4. EXCRETORY PRODUCTS: Waste products of tissue metabolism are carried through blood to respective sites like skin, lungs & kidneys & get excreted.
B. HOMOEOSTASIS:
1. WATER BALANCE: Liquid portion of blood is freely interchangeable with interstitial fluid that helps in the maintenance of its composition, tonicity & pH.
2. OSM.PRESSURE (π) BALANCE: Plasma proteins, especially albumin, maintain colloidal π that helps fluid exchange between blood & tissues. π is expressed in terms of osmolarity & it is about 290 mOsm/L.
3. BODY TEMPERATURE: Regulates body temp. through, (a) high specific heat, (b) high thermal conductivity, (c) high latent heat of vaporization, (d) quick flow (these are due to the properties of water which is the chief constituent of blood).
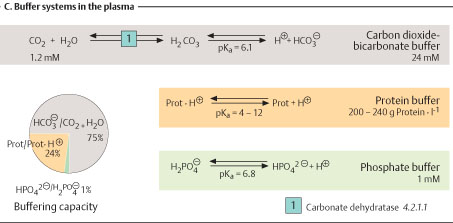
4. ACID-BASE BALANCE: The physiologic pH of the system (7.4) is maintained by blood by its buffering capacity (HCO3, H2PO4, Hb buffers).
5. IRON BALANCE: Haemoglobin in RBC contains 2.5 g (>60%) of the total Fe2+ content of the body (4 g).
6. PROTEIN BALANCE: Blood serves as reservoir of protein & supplies them in terms of amino acids to tissues.
C. DEFENCE:
WBCs present in blood & antibodies that are secreted by activated B-lymphocytes serves as protective mechanism against invading antigens by various mechanism like phagocytosis, complement-mediated lysis, etc.
D. COAGULATION:
Proteases known as clotting factors along with fibrinogen, prothrombin, Ca2+, Vit-K & many other proteins help in blood clotting. Platelets initiate this mechanism. It is accompanied by:
1. Vasoconstriction to prevent blood loss.
2. Sealing of damaged blood vessel to maintain homoeostasis.
PHYSICAL PROPERTIES: Mammalian blood is a thick, viscous, red, opaque fluid.
1. COLOUR: Scarlet red in artery & purple red in vein. Serum & plasma are usually transparent but may appear cloudy or even milky due to fat emulsification. Plasma is yellow due to bilirubin.
2. pH: Physiologic pH is 7.4 maintained within a very narrow range of 7.35-7.45.
3. ODOUR: Freshly drawn blood has a characteristic odour.
4. TASTE: Salty due to inorganic ions.
5. TEMPERATURE: Mean 37.5oC. Blood gets warmed up while passing thro’ muscles & glands & gets cooler on passing thro’ capillaries in homoeothermics.
6. SPECIFIC GRAVITY: It is dependant on the cellular & plasma protein contents. Avg. values:
Whole blood 1.055-1.06 (M); 1.05-1.055 (F)
Plasma 1.025-1.029
RBCs 1.085-1.1
Sp.gr. of foetal blood at full term is highest & that of mother is lowest after birth it rapidly falls due to destruction of RBC.
7. VISCOSITY: Relative viscosities of water, plasma & whole blood are 1, 3 & 5 respectively. It is increased by low temperature, increased formed elements, high blood sugar & calcium content.
8. OSMOTIC PRESSURE (π): Blood exerts about 25 mmHg of osmotic pressure that is entirely due to colloidal proteins of plasma. This value is relatively constant. π when expressed in terms of osmolarity & it is about 290 mOsm/L.
9. SUSPENSION STABILITY & SEDIMENTATION RATE: The rate of settling down is sedimentation rate which is converse to suspension stability (resistance to sedimentation rate). During sedimentation the RBCs adhere to each other to form rouleaux (spell: row-loo). Sedimentation rate is expressed as the height of clear plasma above the packed cell layer in mm/hr.
Normal values of ESR or BSR: Westergren’s method: 0-15 mm/hr (M)
(ref. practicals) 0-20 mm/hr (W)
Significance of ESR : It has great prognostic importance e.g.,
· To assess activity of destructive lesion e.g., TB.
· To assess the activity of inflammatory state in rheumatic infections.
· To differentiate benign & malignant tumor of pelvis.
· To estimate the severity of lesions in pyrogenic infections.
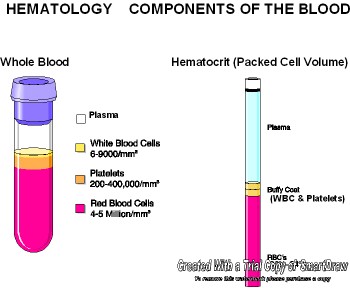
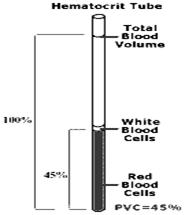
10. HAEMATOCRIT (packed cell volume): PCV is expressed as % of cellular elements with that of whole blood. The value may be affected by centrifugation conditions. Avg. values: (ref. practicals)
40-45% (M); 36-47% (F); Baby 35%; Children (10 yr) 37.5%
11. REACTION: Blood is alkaline (pH 7.35-7.45). The principal H+ ion is CO2. Reaction changes towards acid side in acidosis (6.8) & alkaline side in alkalosis 7.8. pH of venous blood at rest is lower than that of arterial blood by 0.02. pH of RBC is 7.1. Blood reactions can be estimated by electrometric, colorimetric & coagulability (jellification) methods.
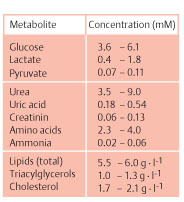
PLASMA
55% of blood. 5% of total body weight. Contains 91% water & 9% solids of which 7-8% is protein & the rest are salts, ions & organic molecules. pH 7.4.
PLASMA PROTEINS: It consists of 4 major fractions [refer table first page]:-
A/G ratio (protein quotient) is roughly 2:1 which remains constant in blood, lymph & transudates of a species. Plasma proteins can be separated by:-
§ PRECIPITATION BY SALTS: Albumin pptd. by fully saturated (NH4)2SO4 solution.
Globulins can be obtained by varying [salt] using MgSO4. The ratio of A/G obtained through salt pptn. is 1.7:1.
§ COHN’S FRACTIONAL PPTN.: 6 types of proteins can be separated by low [salt] at 0oC with varying pH & [alcohol]. They are: 1) fibrinogen & antihemophilic globulin, 2) Isohemagglutinins, PT, fibrinolysins, complement, 3) Angiotensinogen, ALP, Lipoproteins, 4) Ig, 5) albumin, 6) β-globulin & FSH.
§ ULTRACENTRIFUGE
§ ISOELECTRIC POINT: At this pH, proteins behave as zwitter ions & has nil electrophoretic mobility & minimum solubility. They get easily pptd. IEP of Albumin 4.64, α-globulin 5.1, β-globulin 5.6, γ-globulin 6.
§ ELECTROPHORESIS: Albumin has highest electrophoretic mobility towards anode followed by α1-globulin, α2-globulin, β1-globulin, β2-globulin & γ-globulin.
1. ALBUMIN (M.wt. 69,000 D): It is the major fraction of plasma protein.
ü Smallest M.wt.
ü Highest electrophoretic mobility
ü Readily coagulates on heating
ü Water-soluble
ü Less asymmetrical therefore less viscous
ü Exerts 80% of total plasma osmotic pressure due to small size & high concentration. [π α c/size]
ü It helps in transport of lipids, bilurubin, certain drugs & hormones
ü Half-life is 18 days
ü Synthesized in liver (10-12 g/d)
ü Concentrated albumin is used to replenish plasma proteins instead of plasma.
Analbuminaemia and bis-albuminaemia are 2 pathological conditions associated with low serum albumin.
2. GLOBULINS (M.wt. 90,000-13,00,000 D)
§ They are of many varieties & are divided into α1, α2, β1, β2 & γ till now by electrophoresis.
§ α1-globulins (2,00,000 D, IEP at pH 5.06) carries bilirubin, lipids & steroids.
§ β1-globulins (13,00,000 D, IEP at pH 5.12). Can bind metals like Fe (Transferrin) & Cu (Ceruloplasmin). 75% lipids are transported in blood by β1 lipoproteins.
§ γ-globulins (Mean 1,56,000 D, IEP at pH 6). These globulin fractions are concerned with immune reactions. 10-15% of the fraction has M.wt. 10,00,000 D.
§ Glycoproteins, lipoproteins, α1-antitrypsin, haptoglobulin, α2-macroglobulin, fetuin & coagulation factors fall under globulins.
3. FIBRINOGEN (M.wt. 3,30,000-4,00,000 D)
Ø Also a globulin
Ø Easily pptd. by 1/5th saturation of (NH4)2SO4
Ø Coagulable at 56oC
Ø About 6 times more viscous than the same amt. of albumin solution
Ø When thrombin is added to fibrinogen it clots (fibrin)
4. PROTHROMBIN
F Probably a globulin
F Forms thrombin in the presence of Ca2+ & thromboplastin
Agammaglobulinemia is absence of globulin from plasma which leads to lack of immunity to bacterial infections but not viral infections. One genetic type & other acquired type (in nephritic syndrome) are found.
FUNCTIONS OF PLASMA PROTEINS
1. maintenance of colloidal osmotic pressure
2. maintenance of viscosity
3. blood clotting
4. acid-base balance
5. carriage of CO2 & other substances
6. rouleaux formation
7. production of antibodies
8. protein reserve
9. regulation of fluid interchange
10. repair of tissue damage
SERUM: A straw-yellow colour fluid with the same composition of plasma except fibrinogen, PT & clotting factors (II, V & VIII).
PATHOLOGICAL VARIATION OF PLASMA PROTEINS
1. Alteration of plasma proteins can be seen during tissue destructive lesions, hyperparathyroidism, malaria, acute infections.
2. Reduced in extensive hepatic damage, experimental hepatectomy.
3. Albumin fraction is reduced in liver cirrhosis & other hepatic lesions, chronic infections, nephritic syndrome & malnutrition.
4. Globulin fraction is reduced in liver cirrhosis & other hepatic lesions, nephritis, multiple myeloma, leukemia, TB, scarlet fever, chronic infections & collagen-related diseases.
Increase Protein fractions take place relatively in conditions of loss of body water.
Decrease Protein fractions occur in hemorrhage, burns & severe malnutrition.
RED BLOOD CORPUSCLES (OR) ERYTHROCYTES
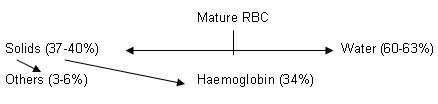
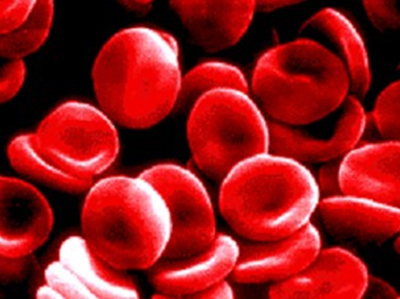
Mammalian RBCs are red, non-nucleated, non-motile, biconcave, discoidal cells.
Without Hb, they appear yellowish.
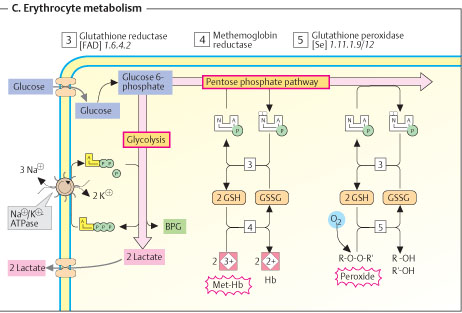
K+ (chief cation), proteins, P-lipids, cholesterol, ATP, 2, 3-BPG, surface Ags, GSH, Enzymes and coenzymes such as carbonic anhydrase, G-6-P DH’ase, GSH peroxidase, GSH reductase, glycolytic enzymes, Catalase, NADPH, etc.
Ø No nucleus, mitochondria, ribosomes, Golgi apparatus or glycogen granules.
Ø No replication, transcription and translation.
Ø Only glycolysis (90%) and HMP shunt (10%) pathways take place.
SIZE: In stained preparation:- Ave. diameter – 7.2 (5.5-8.5) μ;
Thickness (at end) – 2.2 μ; (at centre) - 1 μ
Surface Area – 120 μ2
Venous RBC > arterial RBC, due to imbibition of H2O when pH shifts to acidic.
Macrocytes – larger than normal RBCs.
Microcytes – smaller than normal RBCs.
Anisocytosis – variation in size of RBCs.
SHAPE: Biconcave discoidal. Elongated body with round ends and a constricted middle part. Since, this shape has the maximum surface are in relation to its mass, considerable area are exposed to gas diffusion. RBCs have higher surface area: volume ratio. Greater flexibility is also rendered because of this shape.
Poikilocytosis – deviation from normal shape as in congenital spherocytosis (spherical) and sickle cell anemia (elliptical).
SP.GR: 1.095-1.101 (higher than plasma).
STRUCTURE: A denser outer envelope resembling plasma membrane and a stroma (the colorless part of the cell which remains after Hb leaves the cell on hemolysis) containing Hb. Stroma contains 50% proteins, 40% lipids (lecithin and cephalin in higher amounts) and 10% carbohydrates.
Structural proteins viz., spectrin and ankyrin and surface antigens (glycoproteins known as blood-group substances) are present.
PERMEABILITY: Highly selective.
Impermeable - bigger colloidal molecules and cations like K+, Na+, etc.
Permeable – some crystalloids like urea and anions (Cl-, HCO3-, etc).
FRAGILITY: The tendency to breakdown or disintegrate, discharging its contents in to surrounding fluid. When RBCs are kept in distilled water they break down, known as hemolysis or laking. Fragility of RBCs can be increased by chemical agents, anions, strong alkali, bile salts, acids, saponin, venoms, viral and bacterial agents, etc. (NOTE: Venous RBC is more fragile than arterial RBC)
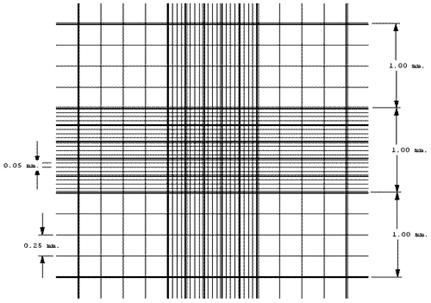
NORMAL RBC COUNT (Neubauer hemocytometer)
Adult male – 4.5-5.6 million/mm3
Adult female – 3.9-5.6 million/mm3
Children (under 1 yr) – 4.5 million/mm3
Children (10 yrs) – 4.7 million/mm3
Infant (cord) – 4-5.6 million/mm3
# RBC < 4 million/mm3 called anemia; RBC > 6.5 million/mm3 called polcythaemia.
ABNORMAL RBC FORMS
Anisocytes, Poikilocytes, Macrocytes, Microcytes, Hypochromic ( [Hb]) and others like:-
 Basophilic
stippling: Stains blue on
Romanowsky staining. Usually occurs in embryo. Increased destruction and new
formation of RBC in post natal life cause this.
Basophilic
stippling: Stains blue on
Romanowsky staining. Usually occurs in embryo. Increased destruction and new
formation of RBC in post natal life cause this.
Howel-Jolly bodies:
Sharply outlined round or angular bodies that are remnants of nuclear chromatin.
Stain with nuclear stains (methyl green).
Heinz bodies: Can be seen when RBC + phenyl hydrazine incubated and stained with methyl violet. Found mostly in hemolytic anemia and can also occur in normal RBCs in the presence of oxidizing reagents.
PHYSIOLOGICAL VARIATION IN RBC COUNTS
RBC due to:
1. Diurnal: Lowest in early hours and highest in later part of the day. Variation is about 4% of mean Hb/day.
2. Meals
3. Muscular exercise: Exercise and other emotional states can cause this rise due to contraction of spleen.
|
ALTITUDE (in thousand metres) |
RBC in million/mm3 |
|
Sea level, 0.2 |
4.25-4.5 |
|
1.3 |
5.2 |
|
2.4-3.6 |
6-6.8 |
|
4.7 |
7.8 |
|
5.5 |
8.3 |
4. High altitude
5. High temperature
6. Infants during first few days of life
7. Males have higher than females
RBC due to:
High pressure (deep mines)
High O2 pressure (>40%)
PATHOLOGICAL VARIATION IN RBC COUNTS
1. Primary polycythemia: a stem cell disorder with increase in RBC, WBC and Platelets. Enlarge spleen. Low serum erythropoietin.
2. Secondary polycythemia occurs in some chronic diseases causing hypoxia e.g.: chronic lung disease, chronic poisoning, and repeated small hemorrhages.
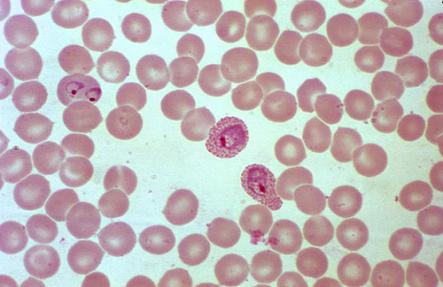
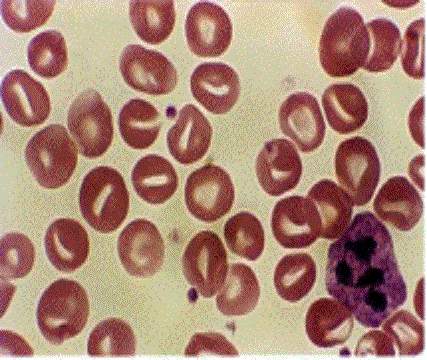
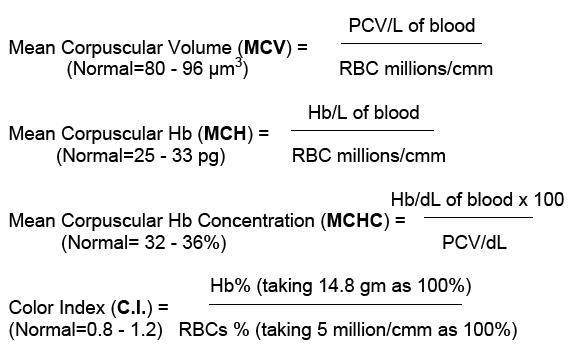
3. Anemia a decrease in red cell count and %Hb below normal level. This may be classified according to size and Hb content of RBC and according to its cause, as follows:
A) Due to variation in size and hemoglobin content:-
Microcytic anemias (hypochromic or normochromic):-
Due to iron deficiency. Reduced Hb leading to low RBC count and decreased size of the RBC. C.I. is lower Eg: About 0.8. MCH, MCHC, MCV is lower. RBC are pale, only colored at the periphery i.e., anisochromia. Response occurs to iron therapy with correction of the causative factor.
Macrocytic anemias (hypochromic or normochromic):-
Deficiency of folic acid and vit-B12 (pernicious anemia or Addison’s anemia). Defect in maturation factors leads to defect in cell division and maturation. Hb is normal. C.I. greater than normal about 1.2 . MCH, MCHC. MCV is greater. Cells are deep red and large size. Response occurs to Vit-B12 (pernicious anemia), folic acid or whole liver extract.
B) According to cause:- [see overall anemia chart next page]
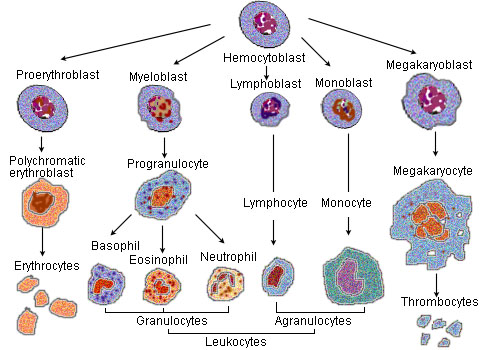
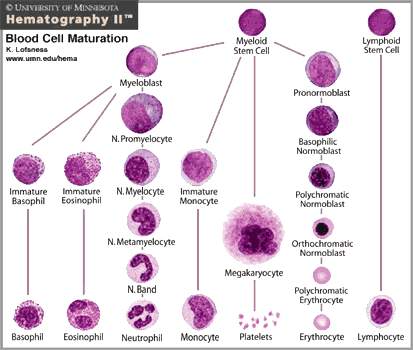
ORIGIN AND DEVELOPMENT OR RBC
Formation of RBCs is known as erythropoiesis which is a continual process. During first and second month of fetal life there are formed in yolk sac, placenta and body stock being developed from endothelial lining of blood vessels. From second to fifth month liver spleen and thymus produce RBCs. In adult, this active red bone marrow is found in sternum, vertebrae, skull, ribs and innominate bones of the pelvis.
|
CELLS |
SIZE |
NUCLEUS |
NUCLEOLI |
CHROMATIN |
CYTOPLASM |
|
Pronormo blast |
15-50 µ |
15 µ |
Multiple |
Thick strands |
Deep violet |
|
Early normoblast |
12-16 µ |
Gets smaller |
Nil |
Coarse and granular |
More basophilic |
|
Intermediate normoblast |
10-14 µ |
Condenses further |
Nil |
Fine |
Less basophilic |
|
Late normoblast |
8-10 µ |
Pyknotic |
Nil |
Fine |
Not basophilic |
|
Reticulocyte |
7-9 µ |
Degenerates |
Nil |
Fine strands |
Light pinkish |
|
Erythrocyte |
6.8-8 µ |
Absent |
Nil |
Nil |
Pinkish |
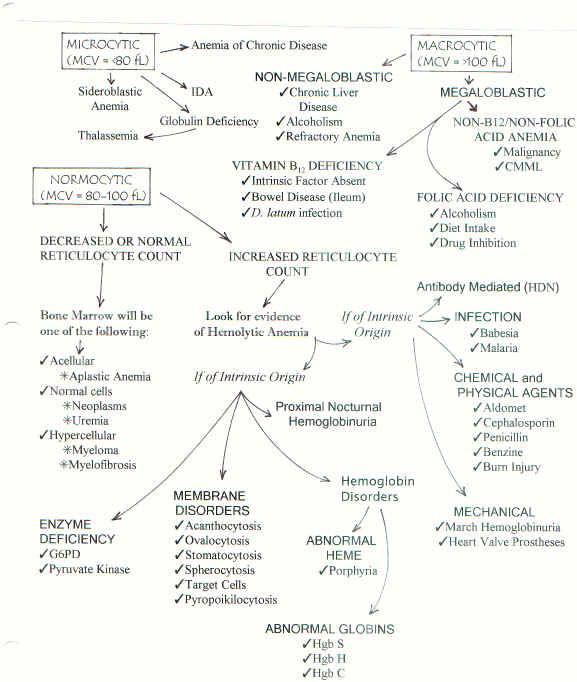
Fig: Various types of anemia)
FACTORS PROMOTING ERYTHROPOIESIS
A) General factors:
B) Hemoglobinization factors:
§ Iron and pyridoxine they are needed to form heme, Vit-C, Co, Mn, and Cu, catalyze this reaction.
§ Porphyrin formed from glycine and succinic acid.
§ Globin synthesized from body proteins.
§ Bile salts facilitates intestinal absorption of metal factors.
C) Maturation factors:
1. Intrinsic factor Vit-B12 (Castle’s hematinic principle), folic acid and Vit-C.
FUNCTIONS OF RBC
HAEMOGLOBIN
Ø Hb is a conjugated chromoprotein forming 95% of solids present in RBCs and imparts color to it.
Ø Hb = Globin (96%) + Heme [4%] (iron and porphyrin).
Ø It has 2 α-chains (141 amino acids each) and 2 β-chains (146 amino acids each).
Ø Each Hb molecule has 4 Fe2+. (1 in each polypeptide chain).
Ø Porphyrin is a pigment with four pyrrole groups. It is a protein, easily crystallizable, water soluble and insoluble in alcohol and ether.
Ø Fe2+ content of Hb is 0.33% which is a constant. On this basis its molecular weight is determined to be 16 kD,
Ø But using ultra centrifuge molecular weight of Hb is found to be 64 kD. Therefore it indicates that 1 molecule of Hb has four Fe2+.
|
MAJOR TYPES OF Hb |
|
|
|
Type |
Subunits |
% present |
|
HbA1 |
α2 β2 |
90 |
|
HbA2 |
α2 δ2 |
< 5 |
|
HbF (foetal) |
α2 γ2 |
< 2 |
|
HbA1c |
α2 β2-glu |
< 5 |
TYPES OF HAEMOGLOBIN
DERIVATIVES OF HEMOGLOBIN
MetHb: It is a true oxide of Hb iron is in Fe3+. It can be obtained treatment with oxidizing agents like K3[Fe(CN)6].
Carboxy Hb: Formed by treating with CO. Cherry red in color. On dilution with water it turns pink (oxy Hb turns yellow).
SulphHb: Formed by passing H2S gas through blood.
MethAlbumin: Heme + albumin. Its presence in plasma indicates hemolysis.
Hematin: Formed by boiling blood with NaOH. This is called alkaline hematin. Water insoluble and soluble in alkali.
Acid hematin: Formed by boiling blood with glacial acetic acid.
Hemochromogen: Formed by denatured globin and reduced heme obtained by boiling dilute blood with NaOH and then adding Na2S2SO4.
Protoporphyrin: Hb on treatment with conc. H2SO4 splits into globin and heme and the latter in turn forms Fe2+ and porphyrin. The porphyrin loses one molecule of water to form protoporphyrin (pink color).
Bilirubin and Biliveridin.
ESTIMATION OF HEMOGLOBIN
HEMATOLOGICAL INDICES: These are useful for determining the type of anemia.
WHITE BLOOD CORPUSCLES (OR) LEUKOCYTES
Leukocytes are nucleated, amoeboid, colorless cells and appear transparent in circulation. The WBC:RBC = 1:700. They develop extravascularly. Rich in nucleoproteins and also contain lipids, glycogen, cholesterol and vit-C along with various enzymes.
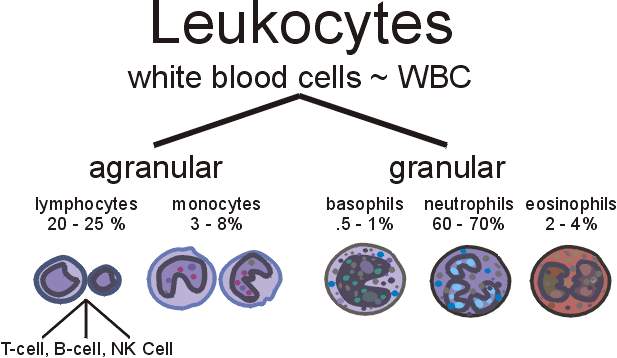

|
TYPE |
SIZE (µ) |
C’PLASM |
GRANULES |
NUCLEUS |
%AGE NO. |
LIFE SPAN |
|
Neutrophils |
10-12 |
Plenty |
Fine, neutrophilic |
1-5 lobed |
60-70 |
4-8 h (blood); 4-5 days (tissues) |
|
Eosinophils |
10-12 |
Plenty |
Large coarse, acidophilic |
2 lobed |
0-4 |
-do- |
|
Basophils |
8-10 |
Plenty |
Large coarse, basophilic |
Kidney-shaped |
0-0.5 |
-do- |
|
Lymphocytes |
8-12 |
Scanty |
None |
Large round |
20-30 |
3 wks-1 yr. |
|
Monocytes |
15-20 |
Abundant |
None, but can show fine ones |
Large, accentric |
2-4 |
Months (tissues) |
|
Thrombocytes |
2-3 |
Abundant |
Fine |
No |
- |
3-10 days |
FUNCTION OF WBCs
Leukocytes are carried in the blood to the body tissue spaces where they perform various functions.
1. Defence mechanism: Phagocytosis (Neutrophils and macrophages), Anti-toxin synthesis, Formation of antibody (Ig) by lymphocytes.
2. Helps in fat metabolism.
3. Blood coagulation.
4. Tissue repair by formation of fibroblasts from lymphocytes.
5. Trephones produced by Monocytes also influences tissue repair and growth.
6. Helps to maintain plasma concentration.
7. Heparin, the anticoagulant in secreted by basophils besides histamine and serotonin.
8. Eosinophils exhibit anti-histaminic activity (anti-allergic).
9. On disintegration they produce Leukocyte Growth Promoting Factor.
WBC COUNT (refer practical)
PHYSIOLOGICAL CAUSES FOR VARIATION IN WBC COUNTS
· Infancy: More lymphocytes (40-60% of TC) than Neutrophils.
· After meals
· Diurnal variation: Rises in afternoon and falls in early morning.
· Leucocytosis (high count) occurs during menstruation.
· In pregnancy and puerperium.
· In muscular exercise.
· In fear, pain and anoxia.
· Injection of adrenaline causes leukocytosis (eosinophilia) along with lymphopenia (low count).
PATHOLOGICAL CAUSES FOR VARIATION IN WBC COUNT
Tissue injury or inflammations attract leukocytes to the site of injury, or inflammation along with increased production of WBCs from bone marrow.
v Pyrogenic Infections: Streptococcal, staphylococcal and pneumococcal.
v Eosinophilia: During allergies, anaphylactic shock, parasitic infections.
v Lymphocytosis: During whooping cough, active TB, malaria, syphilis, E.coli infections, diphtheria, Hodgkin’s disease.
v Monocytosis: During glandular fever, TB, malaria, syphilis, brucellosis and bacterial endocarditis.
v Leukemia: Increases up to 100,000/cmm. Immature type of cells starts to increase. Can be classified in to myeloid, lymphoid or monocytic type depending on the type of cellsinvolved. May be acute or chronic.
v Leukopenia: Less than 4000/cmm. Occurs because of bacterial infections, viral infections, parasitic infections, ACTH or corticosteroids administration, folate deficienry, administration of sulfonamides, benzol, aspirin, DNP, quinine, chloramphenicol, etc., starvation and debilitating conditions, repeated exposure to X-rays, etc.
v Agranulocytosis: Decreased granulocytes (TC < 2000/cmm or even 500/cmm). Drugs that cause leucopenia when used in over doses can cause this. Infectional depression of bone marrow cause this. Characterized by necrotic ulvers in throat, gum and mucous membrane of mouth. Pentose nucleotide injection helps to reverse this condition.
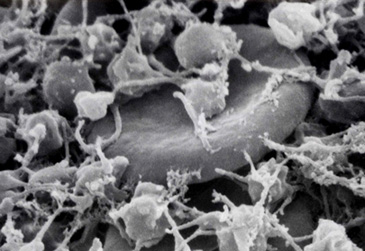
PLATELETS (OR) THROMBOCYTES
a) These are tiny, oval, round (biconvex disk) or rod-like cytoplasmic structures with granules but no nucleus.
b) Formed in red bone marrow from megakaryocytes (their pseudopodia are cut and released in to blood as platelets).
c)
 Their
no. may fluctuate from hour to hour.
Their
no. may fluctuate from hour to hour.
d) They have ABO Ag but not Rh.
e) They are rich in catecholamines.
f) They are destroyed in reticulo endothelial cells in spleen (when splenectomy is done, the lungs take up this job).
g) The cell membrane consists of glycoprotein and mucopolysaccharides.
h) They have microfilaments and microtubules in cytoplasm.
i) The cytoplasmic granules contain lysozyme, lysozyme-like enzymes, glycogen, few mitochondria, Golgi bodies, serotonin and histamine.
PHYSIOLOGICAL VARIATION IN PLATELET COUNT
Increase Count: Diurnal variation, exercise, meals and infections.
PATHOLOGICAL VARIATION IN PLATELET COUNT
Increase Count: Hemorrhage, allergies, myeloid leukemia, surgical procedures and Hodgkin’s disease.
Decrease Count: Purpura hemorrhagica, anaphylaxis, aplastic anemia, pernicious anemia, irradiation and acute infections.
Thrombocytopenia: When count < 30,000/cmm, spontaneous hemorrhage occurs. Bleeding occurs in skin (purpura), mucosa, nose, mouth, GI and urinary tract. In severe cases, bleeding also occurs in optical, fundal and intracranial regions. Coagulation time is normal, but bleeding time is high. Delayed clot retraction and clot is soft.
Thrombocytosis: When count > 400,000/mm3 and in some cases 1,000,000/mm3 (essential thrombocythemia). Bleeding, bruising, arterial or venous thromboses are seen. This may be due to malignant megakaryocyte proliferation or associated with myeloid leukemia or polycythemia vera.
FUNCTIONS
a. One of the chief suppliers of potent coagulation factor, e.g., thromboplastin.
b. Help in clot retraction and squeezes the yellow serum.
c. They seal the leak in blood vessels by their adhesive property.
d. They encircle antigens due to high agglutinating tendency and acts in defense.
e. Secretes serotonin and causes vasoconstriction.
f. Have antigenic properties due to ABO groups and agglutinates causing platelet lysis.
g. Contributes in formation of new endothelial cells, which are damaged during injury.
h. They liberate a protein (?) which increases vascular permeability and contribute to the humoral control of inflammatory reactions.
CONTROL OF THROMBOPOIESIS
F Thrombopoietin, a humoral agent, controls thrombopoiesis.
F The no. of circulating platelets has a feed-back mechanism also.
F Spleen also destroys platelets through RE cells and regulates their circulating amounts.
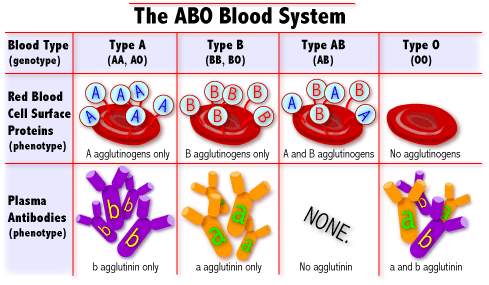
BLOOD GROUPS
Carl Landsteiner (1901) demonstrated that humans could be classified in to 4 groups depending on certain characteristics possessed by their RBCs (ABO system). In 1927, he along with Levine found another distinct blood group system comprising of antigens M, N and MN. In 1940, along with Weiner he discovered Rh factor.
ABO SYSTEM (The Classical Blood Group)
· The antigens (agglutinogens, because they cause agglutination with respective antibody, namely agglutinins-IgM type) that are inherited according to Mendelian law are present in the surface of RBC of humans. They can be grouped as A (42%), B (9%), AB (3%) and O (46%).
· In humans, agglutinogens have reciprocal relationship with agglutinins, i.e., person with Ag-A will have Anti-B antibody, Ag-B will have Anti-A antibody, O will have both anti-A and anti-B antibodies and AB will have both Ag-A and B.
· These antigens are O-linked oligosaccharides (refer: Zubay for chemical composition) that are highly immunogenic.
· A group has A1 and A2 subtypes. Similarly several subtypes were classified.
· Apart from this other rare types like S, P, Lutheran, Lewis, Kidd, Duffy, etc., are found.
To determine the blood group of an individual, a suspension of RBC is made in isotonic saline and is mixed on a glass slide with test serum containing agglutinins and seen for clumping reaction.
BLOOD GROUP COMPATIBILITY
In transfusion, if the blood of the donor and recipient are not compatible, agglutination and subsequent hemolysis of donor’s RBC (that is received) will take place in the recipient leading to disastrous effects.
So, a compatibility testing is done before transfusion. Keep in mind that while doing so, the reaction between donor’s RBC and recipient’s serum alone is taken in to consideration.
This is because serum antibodies of donor are sufficiently diluted by the much larger volume of plasma of the recipient, leading to a less titre value and do not produce any ill effects. Additionally, they are also neutralized by soluble antigens found freely in body fluids.
EFFECTS OF INCOMPATIBLE BLOOD TRANSFUSIONS
Agglutination, hemolysis, jaundice due to hemolysis, Hb’uria, renal failure and death in severe cases.
Rh FACTOR
· When blood from Macaque rhesus (monkey) was injected in to rabbit, antibodies were produced. These antibodies agglutinated the RBCs of monkeys and also humans (85%). This antibody was thus named Rh-antibody (anti-Rh).
· The agglutinating cells are Rh + (they have Rh antigen but not anti-Rh) and those not are called Rh – ve (they do not have either Rh-antigen or anti-Rh normally, but can produce anti-Rh on introducing Rh antigen in them).
· Rh antigens are present only in RBC and do not have secretors as seen in case of ABO.
· Anti-Rh are IgG-type antibodies that can easily cross placental barrier.
· At present 6 Rh Ag are known, viz., C, c, D, d, E, e. Of these, anti-D is abundant and of much clinical importance.
· When Rh + blood is given to an Rh – person anti-Rh develop in 10-12 days, so that only a second transfusion only causes agglutination.
ERYTHROBLASTOSIS FOETALIS (Rh – mother giving rise to a Rh + foetus)
Foetal RBCs or antigenic fragments of foetus may gain accidental entry into maternal circulation (due to placental abnormalities or during time of delivery) evoking Ab response. This anti-Rh from mother enters foetal circulation and agglutinates the foetal RBCs. This condition is known as EBF. The baby may die in utero (hydrops foetalis) or the infant after birth may develop hemolytic jaundice and subsequent abnormalities.
Usually EBF does not affect the first child since the time taken and intensity of response will be negligible. Subsequent carriages of Rh + foetus poses problem in increasing order.
Though EBF is theoretically possible, its occurrence is extremely rare because, IgM antibodies formed usually in mother does not cross the placental barrier. Very rarely, some O-type mothers give rise to IgG antibodies that can cause EBF.
Eventhough Rh incompatibility may occur, there may be difference in ABO groups that can prevent EBF. E.g.: when foetus is A + ve and mother is O – ve, the RBC on entering mother’s circulation will be clumped by anti-A and gets destroyed.
Rh – ve women who have had previous Rh + transfusions can give rise to EBF even during first pregnancy.
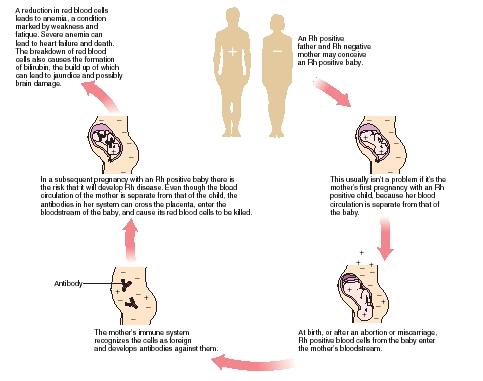
EFFECTS OF EBF
a. Child may be still-born.
b. Can suffer from severe hemolytic jaundice and therefore anemia after birth.
c. Hepato- and splenomegaly are observed.
d. Erythroblasts (not erythrocytes) occur in circulation, i.e., erythroblastosis.
e. Increased bile pigments formation, leading to crossing of unconjugated Bilirubin in the poorly developed BBB of the infant and gets deposited in the basal ganglia (kernicterus) leading to motor disturbances and mental impairment.
PREVENTION OF EBF
Ø Rh – ve mother is sensitized with passive immunization with a serum containing anti-Rh antibody (Rhogam). This is done with 48 h soon after delivery. These Ab circulate in maternal blood for about 3-8 wks and destroy all Rh + factors before the Ag can initiate an Ab response.
Ø Rh – ve women should not be given Rh + transfusion at any time (atleast not before menopause).
SIGNIFICANCE OF BLOOD GROUPS
ü For transfusions
ü For solving paternity disputes
ü Disease linked with ABO groups (e.g.: peptic ulcer believed to occur commonly in O-group people and gastric malignancy in A-group).
ü Anthropological analyses.
ü Establishing identity of subjects, e.g. tracing missing babies in maternity ward.
AUTO-AGGLUTININS: In the absence of Ab, RBC sometimes agglutinates due to auto-agglutinins. They occur in cold and are inactive when temperature is raised.
PAN-AGGLUTININS: Occurs during bacterial infections. They take place in old stored blood and not with fresh samples. They cause non-specific agglutination.
******