FOODS
Foods are substances from animal and plant sources that yield heat and energy when ingested and absorbed by the body. Food nutrients build and renew tissues and regulate body processes.
Diet is the kind and amount of food prescribed for a person or animal for a special reason or food and drink regularly provided or consumed or a regimen of eating and drinking sparingly so as to reduce one's weight.
Healthy eating is about maintaining a balanced diet. This means eating foods from all the different food groups in the right amounts. There are five main food groups, and each one contains nutrients that are essential for your body's growth, energy and body maintenance. Nutrients are vitamins and minerals that regulate your body's chemical processes and functions and help to keep you fit and healthy.
The five main food groups are:
Carbohydrates
Carbohydrates include foods like bread, pasta, potatoes, cereals, low fat oven chips, rice, oats, noodles, couscous, maize and cornmeal. They provide energy and should make up about one third of your diet.
Carbohydrates are divided into two groups - refined and unrefined. Refined carbohydrates include white bread and sugary cereals that have had the fibre removed. Unrefined carbohydrates include brown and wholemeal bread, pasta and rice, and you should choose these options whenever possible.
Some people think starchy foods are fattening. However, it is the fats that are added to them, such as butter and cheese, which can make them unhealthy. Avoid frying these foods and choose healthier alternatives, such as low fat oven chips rather than fried chips.
Fruit and vegetables
Fruit and vegetables are rich in vitamins and minerals which are essential nutrients that your body needs in order to work properly. As well as keeping your skin and hair healthy, they can reduce your risk of getting heart disease and some cancers.
You should aim to eat five portions of fruit and vegetables each day. They can be fresh, frozen, canned or dried. One portion counts as a large piece of fruit, such as an apple or banana, three heaped tablespoons of vegetables, or one glass of 100% fruit or vegetable juice (although this only counts as one portion regardless of how much you drink). Beans and pulses, such as baked beans or lentils, also contribute to this group, but they only count towards one portion no matter how many different types you eat.
Protein
Protein helps to build and repair your body. Foods rich in protein also contain minerals, such as iron, zinc and magnesium, as well as important B vitamins. They should make up about one fifth of what you eat each day.
Sources of protein include meat, fish and eggs, as well as non-animal products, such as beans and nuts. To keep it healthy, trim fat from meat, remove the skin from chicken, drain fat away after cooking, and try to eat two portions of fish each week. One of these fish portions should be oily fish, such as salmon, mackerel or fresh tuna. Canned tuna does not count as oily fish because the canning process removes the beneficial oils. Avoid frying meat and fish, and try to grill, roast or microwave instead.
If you are a vegetarian, you can get the protein that you need by including seeds, nuts, tofu, soya products and beans in your diet. These foods provide protein, fibre and iron but, unlike the non-vegetarian examples, they do not provide much zinc or vitamin B12 unless they are fortified (have had vitamins or minerals added to them).
Dairy
Cheese, milk, yoghurt and calcium fortified soya alternatives are all examples of dairy foods (cream and butter are in the fats group, and eggs fall under protein). Dairy products are rich in calcium, which is important for strong bones and teeth. You should aim to get 700mg of calcium each day, which is roughly the same as a pint of milk, or two small yoghurts. Choose lower fat versions, such as semi-skimmed milk, low fat yoghurt and reduced fat cheese.
If you do not drink cow's milk or eat dairy products, you can get calcium from soya milk and yoghurts with added calcium, and from vegetables such as broccoli and cabbage.
Fat and sugar
Fats and sugars contain more energy than any other food group and should make up the smallest part of your diet. Foods such as butter, mayonnaise, chocolate, crisps, cakes, soft drinks, jam, sweets and ice cream, all usually contain high amounts fat.
Fats are divided into two groups - saturated and unsaturated. Saturated fat is found in cream, margarine, and fried foods. This type of fat can contribute to heart disease. Unsaturated fat is found in vegetable oils and oily fish. Eating a small amount of unsatuated fat will help to keep your immune system healthy and can reduce cholesterol levels.
Sugary foods are bad for your teeth and are full of calories. You should therefore eat them sparingly, as a special treat.
Guide to Food Eating
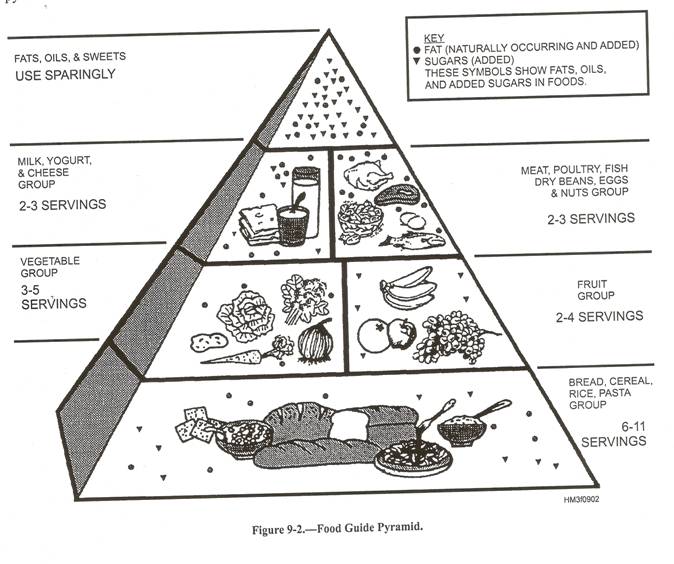
Calculating a therapeutic diet can be complicated and is best left to dietitians. It is now common practice for dietitians or dietary kitchens to select foods for diets using the food groups outlined in food guide pyramid. These foods are classified according to their nutritional value and the number of servings that should be eaten each day.
Food Guide Pyramid
The food guide pyramid emphasizes foods from the five food groups shown in the sections of the pyramid. Each of these groups provides some, but not all, of the nutrients we require. For good health we need them all. For everyday living, the simplest and most practical plan is to follow those same guidelines, selecting from the various food groups the type and amount of food recommended.
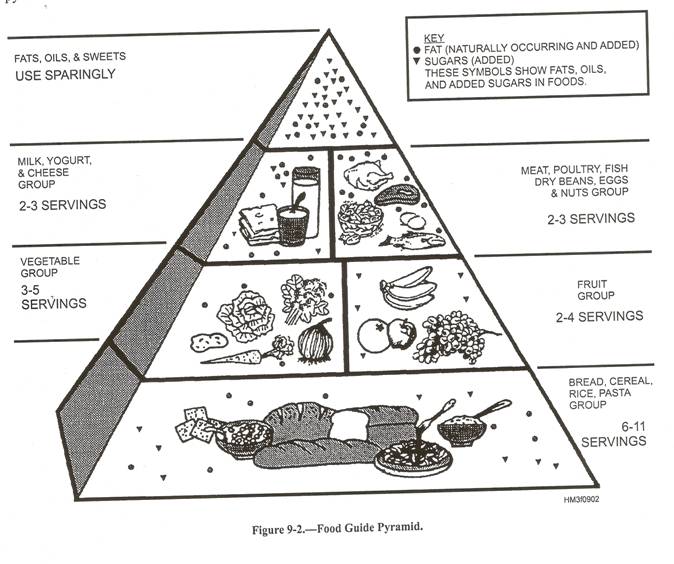
Dietary Guidelines:
These recommendations are as follows:
! Eat more grains, vegetables and fruits
! Eat moderate amounts of lean meats and dairy foods
! Use sweets, fats and oils sparingly
Generally accepted guidelines suggest that you eat a diet that is high in complex carbohydrates and low in protein and fat. Your diet should consist of at least five combined servings of fruits and vegetables each day. Avoid fat when possible. Eat at regular intervals when possible and avoid snacking late at night.
Diet therapy:
Diet therapy is the diet planned by adjusting the quantity and quality of food intake to improve health status of an individual. This term does not include the methods of food intake. Diet therapies are specially designed and prescribed for medical and/or general nutritional reasons.
Purpose
Diet therapy promotes a balanced selection of foods vital for good health. By combining foods appropriate for each individual and drinking the proper amount of water, one can help maintain the best possible health. Eating the proper diet is critical for the health of individuals, groups with special medical and dietary needs, and entire populations afflicted with malnutrition.
Precautions
A particular modified diet is prescribed specifically for each individual. Those individuals who have medical conditions or who are sensitive to certain foods need to be very compliant and cautious about what they eat.
Objectives of Diet Therapy:
The objectives of diet therapy are as follows:
o To increase or decrease body weight
o To rest a particular organ
o To adjust the diet to the body’s ability to use certain foods
o To produce a specific effect as a remedy (e.g. regulation of blood sugar in diabetes)
o To overcome deficiencies by the addition of food rich in some necessary element (e.g. supplementing the diet with iron in treating macrocytic anemia
o To provide ease of digestion by omitting irritating substances, such as fiber, spices or high fat foods
Types of Diets:
There are usually two types of diets namely regular diet and modified or therapeutic diets.
Regular Diet:
The regular diet is composed of all types of foods and is well balanced and capable of maintaining a state of good nutrition. It is intended for convalescing patients who do not require a therapeutic diet.
Modified or Therapeutic Diets:
Modified or therapeutic diets are modifications of the regular diet and are designed to meet specific patient needs. These include:
Ř Method of preparation (e.g. baking, boiling or broiling)
Ř Consistency (e.g. ground or chopped)
Ř Total calories (e.g. high or low calorie)
Ř Nutrients (e.g. altering carbohydrate, protein, fat, vitamins and minerals) and
Ř Allowing only specific food (e.g. diabetic diet)
Different therapeutic diets shown in the following table:
|
S.No |
Diet Name |
Diet |
Disease |
|
1. |
Soft Diet |
It is soft in texture and consists of liquids and semi-solid foods. |
Postoperative cases, acute illnesses and gastrointestinal disorders |
|
2. |
Liquid Diet |
It consists of foods that are in a liquid state at body temperature |
Postoperative cases, acute illnesses and gastrointestinal disorders |
|
3. |
High Calorie Diet |
It is of a higher caloric value than the average patient normally requires |
Malnourished, Underweight, postsurgical or convalescing patients |
|
4. |
High Protein Diet |
It is rich in Protein which is essential for tissue growth and regeneration |
Nephritis, Cirrhosis, Infectious hepatitis, Burns, Fractures |
|
5. |
Low Calorie Diet |
It consists of low calorie i.e. 1,000 to 1,800 calories per day |
Arthritis, Hypertension, Diabetes, Cardiac disease and Hypothyroidism |
|
6. |
Low Protein Diet |
It is made up of foods that furnish only small amounts of protein and consists largely of carbohydrates and fats. |
Renal diseases and Liver disorders |
|
7. |
High Residue Diet |
It consists of rich in fiber foods like whole-grain breads and cereals, fruits and vegetables |
Spastic colon, irritable bowel syndrome and diverticulosis |
|
8. |
Low Residue Diet |
It is simple diet which can be easily digestible and provide less fecal content |
Ulceration, inflammation other gastric disorders |
|
9. |
Low Sodium Diet |
It consists of foods containing a very small percentage of sodium, with no salt added in preparation or by the patient |
Edema is present in renal disease, hypertension and certain cardiac conditions. |
|
10. |
Bland Diet |
It consists of foods that are not irritating GI tract. |
Gastritis, Hyperacidity, hemorrhoids, pepetic ulcers and other GI disorders |
CANCER DIET PLAN:
Doctors and dietitians should be constantly aware of the diagnostic significance of loss of weight, anorexia and food aversions as early signs of malignant disease. When the diagnosis has been made and a programme of ablative surgery, radiation or treatment with cytotoxic drugs laid down, a supportive diet should be carefully drawn up. This should be higher than normal in energy and nutrient content and in a form which is acceptable and appetizing to the patient while avoiding any food aversions he may have. Many patients require supplementary and tube feeding and some parenteral nutrition.
Dietary modifications may be necessary as a result of ileostomy and colostomy. There is no evidence that a good diet can cure any type of cancer but there is no doubt, that it can ad greatly to the comfort of the patient. Since the ultimate hope for the patient may lie in a strong immune reaction to the invading tumor cells and since there is evidence that a good diet supports the immune system, a rational basis for diet therapy is at least dimly perceptible.
For the most part, however, good diet therapy supports the patient’s morale; it provides normal pleasurable gratification of the body and mind when these are being restricted by advancing disease. Great care should therefore be taken about the aesthetic aspects of the diet, such as arrangement, appearance, odour or bouquest and taste of the foods.
Eight Point Plan:
1. Be as lean as possible. Aim for Body Mass Index of 21 - 23.
2. Be Active. Aim for 60 minutes or more moderate activity every day, or 30+ minutes of vigorous activity.
3. Avoid energy-dense foods and sugary drinks. Avoid foods that are high in fat, like fast foods and processed foods. Also avoid sugary drinks like soda.
4. Eat plant-based foods. Aim for 5 servings of non-starchy fruits and vegetables every day (potato, yam, sweet potato, and cassava don't count). Eat only limited amounts of refined grains like white bread and pasta. Instead, include legumes or whole grains in every meal.
5. Limit red meat and avoid processed meat. Limit red meat intake (beef, pork, lamb and goat) to less than 18 oz. a week and avoid processed meat at all costs.
6. Limit alcohol. Men: no more than 2 drinks a day. Women: no more than 1 drink a day
7. Limit salty foods. Salt and salt-preserved foods are probably a cause of stomach cancer. Limit sodium intake to 2400 mg a day
8. Don't bank on pills. Some supplements or high-dose nutrients are associated with higher risk of developing cancer. Stick to a healthy diet instead and don't bank on dietary supplements as the magic pills in preventing cancer.
DIETARY PLAN FOR CARDIO VASCULAR DISEASE (CVD):
Diet Principles:
The following dietetic suggestions are useful for the prevention and treatment of CVD.
1. Restrict total calories to reduce body weight and maintain it at the normal for height, age and sex.
2. It is not desirable to restrict all forms of fats, as severe restriction results in mental and physical depression.
3. Fats should form 30% of the total calories
4. Fats should be consumed partly as unsaturated vegetable oils such as cottonseed, groundnut oil and olive oil.
5. Saturated fats, hydrogenated vegetable oil (vanaspathi), margarine and animal fats like butter, ghee and the fat of animal meat should be taken in moderation.
6. Green vegetables, fruits, cereals, skimmed milk, and lean meat can be taken liberally. Sugar intake should be reduced.
7. Three or four small meals are preferable to two big meals. The evening meal should be about two hours before sleep.
8. Regular exercise is most useful, but physical strain after a meal should be avoided.
9. Smoking should be stopped and alcohol should be stopped or minimized.
Sample Menu (Low Fat, High complex Carbohydrate Diet)
|
Western Diet |
|
Vegetarian Diet |
|
Fruit Juice Whole grain with skimmed milk Wholemeal bread/toast Tea or coffee |
Break fast |
Fruit Juice Puffed rice with skimmed milk Wholemeal bread/toast Tea or coffee |
|
Tea or coffee Fruit |
Mid-Morning |
Tea or coffee Fruit |
|
Poached cod Peas Croquette Potatoes toast Low fat Yoghurt/curd |
Lunch |
Lentil Soup Cottage cheese Rice pudding or chapattis with little ghee cooked brinjals Rice and dal |
|
Tea or coffee Wholemeal biscuits |
Mid-afternoon |
Tea or coffee Plain biscuits |
|
Clear Soup Roast chicken Broad beans or roast potatoes Fresh fruit |
Dinner |
Leek Soup Pasta in sauce Vegetable Salad Dosa and sambhar / chutney Strawberry jelly |
DIETARY PLAN FOR DIABETES MELLITUS (DM)
Diabetic diets aim to restrict carbohydrate intake while meeting normal needs for protein and providing just sufficient energy to maintain normal weight in adults and to allow for growth in children. A moderate to high intake of dietary fibre is also advocated. Diets are made up from lists of exchanges, quantitatively defined. Different systems of exchanges are used by the British and American Dietetic and Diabetic Associations. The British Associations use carbohydrate exchanges; formerly protein and fat exchanges were also used but these are no longer recommended officially. The American Association use bread, milk, fruit and vegetables exchanges.
Constructing the Diet
Each carbohydrate exchange contains approximately 10g carbohydrate with an energy value of about 50kcal (equivalent to 20g bread). One pint of milk contains approximately 30g carbohydrate with an energy value of about 380kcal. Thus a diet prescription for 180g carbohydrate, 1800kcal would be calculated as follows:
1. The daily intake of carbohydrate (180g) represents 18 carbohydrate exchanges.
2. The daily allowance of milk is decided either on the basis of patient’s food habits or on his special requirements. For example 1 pint milk contains 3 carbohydrate exchanges.
3. These provide 900kcal (18 exchanges) and the remainder of the energy provided by protein and fat. At least 10% of the energy has to come from protein.
4. Finally the carbohydrate exchanges are distributed throughout the day according to the eating habits and daily routine of the patient and the insulin regimen.
Plan of Distribution
Breakfast 4 carbohydrate exchanges
Butter and milk for allowance
Tea or coffee (no sugar)
Mid-morning 1 carbohydrate exchanges
Butter and milk for allowance
Tea or coffee (no sugar)
Midday meal Clear soup if desired.
4 carbohydrate exchanges
Vegetables if desired
Butter and milk for allowance
Mid-afternoon 1 carbohydrate exchanges
Butter and milk for allowance
Tea or coffee (no sugar)
Evening meal 4 carbohydrate exchanges
Vegetables if desired
Tea or coffee (no sugar)
Bedtime 1 carbohydrate exchanges
Remainder of butter and milk for allowance
Allowance for day: 1pint (560ml) whole milk
30g butter or margarine
Sample Menu
Breakfast 120g porridge with milk from allowance
60g wholemeal bread with butter from allowance.
Tea or coffee with milk from allowance.
Mid-morning 15g low sugar biscuits
Tea or coffee with milk from allowance
Midday meal Clear soup with shredded vegetables
Lean Meat or fish or egg or cheese
120g boiled potatoes
120g orange
Small carton of low fat yogurt
Milk from allowance with coffee
Mid-afternoon 15g wheatmeal biscuits
Tea or coffee with milk for allowance
Evening meal Meat or fish or egg or cheese
Unrestricted vegetables
60g wholemeal bread with butter from allowance
120g raw applet
Tea or coffee with milk from allowance
Bedtime Remainder of milk from allowance
20g bread and butter from allowance
ULCER DIET
In general, the dietetic therapy of gastric and duodenal ulcers, gastritis and non-ulcer dyspepsia is similar. There were nearly 20 dietary regimens advised; obviously such scrupulous diet control is not necessary. Dietary treatment should be relatively simple to the patient. Almost all foods are permitted in moderation, except chillies and sour food. Chillies, meat soups and extractivities increase peptic pain and should be avoided. Sour foods and unripe citrus fruits aggrevate peptic discomfort. Restricted use of garlic, ginger, coriander and cumin seeds to the flavor of food and makes it appetizing. Fats such as oil and ghee are permitted in cooking, but fried food which is normally difficult to digest is restricted. Smoking, tobacco chewing and alcohol also perpetuate the symptoms.
A snack or meal every three hours is probably the most important aspect of dietary therapy. Duodenal ulcer patients secrete less gastrin on small six-hourly feeds than with three big meals. The spontaneous cure rate of peptic ulcer reported from many centers, is probably because patients admitted to hospital receive three meals at regular hours plus snacks at mid-morning and afternoon. The Indian diet, both in hospital and at home, almost always contains chillies, which need to be restricted. Milk always been known to relieve pain in peptic ulcer.
Sample Menu:
|
Western Diet |
|
Vegetarian Diet |
|
Cornflakes Scrambled egg Tea or coffee |
Break fast |
Porridge Tea or coffee |
|
Milk drink Plain biscuits |
Mid-Morning |
Milk drink Plain biscuits |
|
Minced meat Mashed Potatoes Sliced carrots or jelly |
Lunch |
Cauliflower cheese Mashed potatoes Lentil curry and rice |
|
Tea or coffee Bread and butter |
Mid-afternoon |
Tea or coffee Cheese sandwhich |
|
Steamed fish Peas creamed potatoes Jelly |
Dinner |
Baked potato With filling Khichdi and Kadhi |
|
Cocoa in milk |
Bed time |
Hot chocolate |
MALNUTRITION (KWAHORKOR, MARASMUS (PROTEIN ENERGY MALNUTRITION OR PROTEIN CALORIE MALNUTRITION))
Protein-energy malnutrition is a comprehensive term; in its advanced form the condition includes marasmus which is a dry form with extreme emaciation and kwashiorkor with water retention (edema). The intermediate type is called marasmic-kwashorkor. Marasmus represents deficiency of protein as well as calories (energy), with severe growth retardation, well-preserved metabolic processes and adequate suprarenal function. Kwashiorkor occurs with deficient protein but relatively adequate calorie supply and breakdown of hormonal adaptive processes, resulting in a characteristic biochemical and clinical picture.
The treatment consists of supplying adequate calories and proteins and of eradicating any infection that may be present. The sensible approach is not doling out elaborately processed and expensive protein-rich formulations, but educating the poor rural communities on the use of locally available cheaper foods like milk, bread, butter, bananas, wheat flour, ghee and cotton-seed flour etc.,
Sample Menu
|
Western Diet |
|
Vegetarian Diet |
|
Fruit Juice Cornflakes Bread/toast Butter and jam or eggs and bacon Tea or coffee |
Break fast |
Fruit Juice Flaked rice Chapatties Tea or coffee |
|
Tea or coffee Biscuits |
Mid-Morning |
Tea or coffee Bread |
|
Roast lamb Minted Peas Roast Potatoes with cheese Salad Apple |
Lunch |
Baked Jacket potato or chapattis Lady’s finger Rice and dal Fruit |
|
Tea or coffee Cake |
Mid-afternoon |
Tea or coffee Nuts |
|
Clear Soup Smoked fish with egg sauce Cabbage rice Jelly and custard |
Dinner |
Leek Soup Vegetable Curry and boiled potatoes Idly with sambhar / chutney or Rice pudding |
JAUNDICE (VIRAL HEPATITIS)
The dietary treatment of viral hepatitis has passed through various phases of evolution, because of conclusions drawn from observations in small series of cases without proper controlled study. Extensive studies among army personnel have shown that patients eating diet supply 3000kcal and 150g protein, supplemented with vitamins, improved more rapidly than those who ate only what they chose. In a 60kg patient with hepatic pre-coma and coma, 1500-2000 kcal should be supplied. Protein containing foods are withheld and only high-carbohydrate containing foods are given. Fatty diet should be restricted in jaundice condition. Carbohydrates are necessary to provide calories and reduce the endogenous breakdown of proteins. Required amount of minerals should be given in the diet.
Food items for Sever Jaundice (Total serum bilirubin > 15mg%)
Permitted:
Bread or chapattis of wheat, rice, maize, jowar, bajra or ragi
Breakfast cereal of wheat, rice, oatmeal or maize
Rice
Milk or milk products
Soups
Vegetable salad
Vegetables cooked
Potato, sweet potato or yam
Fruits, fresh and dried
Sugar, Jaggery or honey
Jam or murabba
Pastry only as biscuits
Desserts as light custard or ice-cream
Beverages, water
Excluded:
Pulses or beans
Meat, fish or chicken
Eggs
Fat for cooking and butter
Nuts
Condiments and spices
Papad, chutney or pickles
Sample Diet menu for Severe Jaundice
Vegetarian and mixed diet
Constituent Amount
Proteins 40g
Fats 26g
Carbohydrates 318g
Calories 1670kcal
Breakfast
Cornflakes (1cup) with skimmed milk (1/2 cup)
And honey or sugar ( 2 teaspoons)
Toast, Banana, Tea or coffee
Mid-morning
Fruit juice (1cup)
Lunch
Mixed vegetable soup
Mashed potato
Cooked French beans or vegetables; baked or stuffed tomatoes
Brad or chapattis
One orange or four dates
Mid-afternoon (3.30pm)
Tea
Biscuits or cream wafers
Evening (6.00pm)
Sugar cane or orange juice (1cup)
Dinner
Tomato soup (1cup)
Butter milk (1cup)
Cooked or creamed spinach
Bread, 2 slices; or khakhra 4
Light custard, ˝ cup
Food items for Mild to moderate Jaundice (Total bilirubin < 15mg%)
Permitted:
Bread or chapattis of wheat, rice, maize, jowar, bajra or ragi
Breakfast cereal of wheat, rice, oatmeal or maize
Rice
Pulses or beans as thin dal 1 cup
Meat, fish or chicken
Egg
Milk or milk products
Soup as thin soup
Vegetable salad
Vegetable cooked
Potato, sweet potato or yam
Fat for cooking and butter (fried food excluded)
Sugar, Jaggery or honey
Jam or murabba
Pastry as biscuits
Sweetmeat
Fruits fresh and dried
Beverages, water
Excluded:
Nuts, Condiments and spices
Papad, chutney or pickles
Sample Diet Menu for Mild to Moderate Jaundice:
|
Mixed Diet |
|
Vegetarian Diet |
|
Proteins 78g Fats 59g Carbohydrates 313g Calories 2100kcal |
Constituents |
Proteins 60g Fats 57g Carbohydrates 348g Calories 2100kcal |
|
Fruit Juice Cornflakes 1 cup with skimmed milk ˝ cup and jaggery (2 teaspoons) Half boiled eggs (2) Toast with Butter Four fresh figs or one orange Tea or coffee |
Break fast |
Puffed Rice 1 cup with skimmed milk 1 cup or honey (2 teaspoons) Toast (2) with Butter (2 teaspoons) Jam (1 teaspoons) One apple Tea or coffee |
|
Fruit juice or sugar cane Juice 1 cup |
Mid-Morning |
Fruit juice or sugar cane Juice 1 cup |
|
Roast mutton or baked chicken with tomato sauce Boiled potato Mixed vegetable salad or tossed salad Cooked or creamed spinach or Broccoli bread (slice) or chapattis (2) Guava or Apple |
Lunch |
Curd 1 cup Thin dal 1 cup or osplit peas soup Rice 2 tablespoons or baked rice ring Cooked pumpkin ˝ cup or Italian vegetable medley Chapatties (4) with butter (2 teaspoons) Banana |
|
Tea Biscuits (4) or Cake |
Mid-afternoon |
Tea Biscuits or Cake |
|
Minced meat (3 tablespoons) or beef stew Baked sweet potato or rice Boiled French beans or braised cabbage Bread (2 slices) or chapattis (4) Rice pudding 1cup |
Dinner |
Butter milk 1 cup Boiled potato or hashed brown potatoes Cooked cauliflower or mushroom stuffed egg plant Khakhra (4) with butter (2 teaspoons) Grapes or stewed apricots |
CIRRHOSIS
A nutritive high protein diet is the most essential part of therapy for liver cirrhosis. Protein rich foods help regeneration of the liver and formation of albumin and serve to combat anemia and ascites. About 80-100 g proteins must be consumed daily. Eggs and flesh foods are excellent but expensive. Relatively inexpensive protein-rich foods are skimmed milk or its powder, dried beans and pulses, chana, groundnuts, cereal preparations, chapattis, khakhras and biscuits. These are best utilized when teaken as a combination during each meal. Thus, a combination of bread, pulses, milk and groundnuts at each meal is better for protein synthesis than eggs or meat alone. Protein rich foods are temporarily withheld if the patient deteriorates into a pre-comatose state. Multivitamin oral preparations are of value. A hematinic tablet containing iron, folic acid, and vitamin B12 is advised. Sodium intake is restricted in patients with cirrhosis and ascites; not more than 3g salt per day is permitted. Cirrhotics without ascites do not require sodium restriction.
Sample Menu for Cirrhosis:
|
Mixed Diet |
|
Vegetarian Diet |
|
Proteins 95g Fats 90g Carbohydrates 280g Calories 2390kcal |
Constituents |
Proteins 75g Fats 85g Carbohydrates 320g Calories 2340kcal |
|
Cornflakes 1 cup or rice crispies Lite boiled eggs (2) 2 Toast with Butter Tea or coffee |
Break fast |
Toast (2) with Butter (2 teaspoons) Jam (1 teaspoons) Tea or coffee |
|
Fruit juice Juice 1 cup |
Mid-Morning |
Fruit juice Juice 1 cup Peanuts (20) |
|
Roast Pork with gravy Medium Boiled potatoes Cooked or creamed spinach or Sweetcorn Baked sponge and custard |
Lunch |
Minestrone Vegetable lasagna Chapatties Cauliflower Rice and dal Banana |
|
Tea or coffee Fruit Cake |
Mid-afternoon |
Tea or coffee Chocolate cream Biscuits 2 |
|
Poahed cod Braised cabbage Rice pudding 1cup |
Dinner |
Cheese and onion flan Creamed Potatoes Carrots Bread and butter or Khakhra with ghee Khichdi with kadhi Icecream |
|
|
Bed time |
A glass of milk |
NEPHRITIS (KIDNEY DISEASES)
There are two types of nephritis namely type-1 and type-2 nephritis.
Type – I Nephritis:
It is otherwise known as acute nephritis or acute glomerulonephritis, characterized by red blood cells and casts in the urine, scanty urine, swelling of the body and high blood pressure.
A low-protein, high-carbohydrate, low-sodium and low-potassium diet with restricted fluids is prescribed. The food mainly consists of cereals, boiled vegetables and milk. The total calorie intake should be about 1700kcal.
The intake of proteins is reduced to a minimum by excluding protein-rich foods. During the acute phase, if urine stops, protein-containing foods should be avoided and 10-20% glucose can be given either orally or through an intragastric drip. When urine flow recommences, the protein intake is increased to 20-30g daily. If the urine passed is 500-700ml, about 0.5g protein per kg body weight is allowed. With free flow of urine, the daily intake is increased to the usual of about 60g. Prolonged restriction of protein leads to weakness and anemia.
The end-products of metabolism of fats do not depend on the kidneys for their excretion, and so fats can be administered. The main source of carbohydrates is cereals. Vitamin C 100mg three times a day, should be given, as deficiency has been noted in acute nephritis. Vitamin-B complex is also useful. The normal kidneys under hormonal control automatically regulate sodium and potassium needs of the body. In acute nephritis, the kidneys are unable to excrete sodium and potassium and so the body electrolyte balance is disturbed. When edema subsides, the intake of sodium as common salt is gradually increased. Potassium should be restricted when there is a scanty flow of urine. Vegetables should be chopped and boiled with excess of water which is drained off to decrease potassium content. Fruits too have high potassium content and are therefore excluded.
Sample Menu:
|
Western Diet |
|
Vegetarian Diet |
|
Cornflakes 1 cup Bread / Toast (1slice) Jam / Margarine Tea |
Break fast |
Bread / Toast (2slice) Jam / Margarine Tea |
|
Tea Plain Biscuits |
Mid-Morning |
Tea Cream crackers (3) |
|
Poached cod (2 oz) Boiled potatoes Boiled French beans Jam sponge cake Aubergines |
Lunch |
Lentile pie (8 oz) Boiled Potatoes or parathas (2) Rice (4 oz) and dal (4 oz) Tinned pears |
|
Tea Crispbreads (2) |
Mid-afternoon |
Tea Plain Biscuits (2) |
|
Chicken casserole (2 oz) Mashed potatoes Sweet corn Apple tart |
Dinner |
Mixed cooked vegetables Creamed potatoes or khichdi (8 oz) And kadhi Rice pudding |
Type – II Nephritis:
Nephrotic syndrome characterized by gradual onset of body swelling with massive protein loss in the urine. Complete recovery is infrequent. There is usually no retention of nitrogenous waste products in the early stages. The total quantity of urine excreted may be normal. Nephrotic syndrome is defined by excretion of morethan 3.5g of protein per day in the urine; serum albumin concentration below 30g per litre; total serum protein below 60g per litre; raised serum cholesterol value and presence of edema without any other apparent cause.
The total calorie intake will be 2000kcal per day. A high protein diet containing at lest 1.5-2g protein per kg bodyweight is adivised. A relatively cheap source of protein is skimmed milk powder, which can be taken with fruit juice or mixed with flour to make chapatties. Concentrated protein foods are also available in the market. Groundnuts and pulses including Bengal gram are palatable, inexpensive protein rich foods.
The usual quantity of fats, 1g per kg, is advised. After the daily needs of proteins and fats are satisfied, the remaining calories are supplied by carbohydrates. Vitamin C, 100mg three times a day, and vitamins of the B group may be given as supplements. Retention of sodium in the body produces water retention (edema). A low sodium diet is helpful during the edematous stage. A convenient method of restricting sodium is to avoid salt in cooking and also at the table. Foods to which salt has been added, such as salted butter, biscuits, and preserved meat fish are excluded. When the edema subsides, a moderate intake of salt is permitted.
Sample Menu:
|
Mixed Diet |
|
Vegetarian Diet |
|
Proteins 118g Fats 68g Carbohydrates 228g Calories 2000kcal |
Constituents |
Proteins 110g Fats 72g Carbohydrates 252g Calories 2100kcal |
|
Cornflakes 1 ˝ up or Shredded wheat with skimmed milk 1 cup and sugar 2 teaspoons Eggs poached 2 or egg mushroom omelette 1 Toast or chapatties 2 Tea or coffee |
Break fast |
Porridge, 2/3 cup with milk 1 cup and sugar 2 teaspoons Cottage cheese, 2 tablespoons Bread 1 slice or khakhra 2 Tea or coffee 1 cup |
|
Skimmed milk 1 cup Banana 1 |
Mid-Morning |
Skimmed milk 1 cup with Skimmed milk powder, 2 tablespoons |
|
Tomato salad Minced meat, 4 tablespoons Cooked pumpkin or cabbage Rice 2 tablespoons or 2 tablespoons rice pulao Bread 1 slice or chapatties 2 Walnuts 4
|
Lunch |
Butter milk 1 cup Vegetable salad Cooked brinjals Rice 2 tablespoons Dal 1 cup Bread 2 slices or chapatties 4 Groundnuts 15
|
|
Tea or coffee 1 cup
|
Mid-afternoon |
Tea or coffee 1 cup
|
|
Fish baked, 1 helping or tuna salad Roast leg of chicken or spare ribs Potato 1 mashed with 1 teaspoon butter Cooked cauliflower Bread 1 slice or chapatties 2 Bread pudding ˝ cup or jam tart |
Dinner |
Cottage cheese, 3 tablespoons Curd, 1 cup Cooked spinach 2 tablespoons Dal 1 cup Bread 1 slice or khakhara 2 |
|
Skimmed milk 1 cup |
Bed time |
Skimmed milk 1 cup with skimmed milk powder 2 tablespoons |