RESPIRATION is the process of gaseous exchange between an organism and its environment. Gaseous exchange between tissues and internal environment is termed as internal respiration, and that between the body and outer environment is termed as external respiration or simply breathing. There are 2 parts in respiration:-
Inspiration or intake of air is an active and dominant act brought about by active muscular contractions, while expiration (breathing out) is passive.
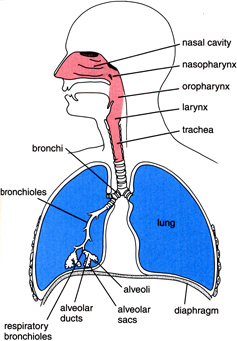
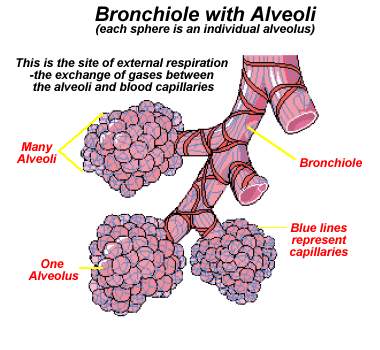
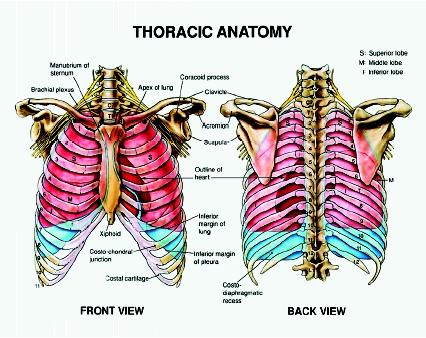
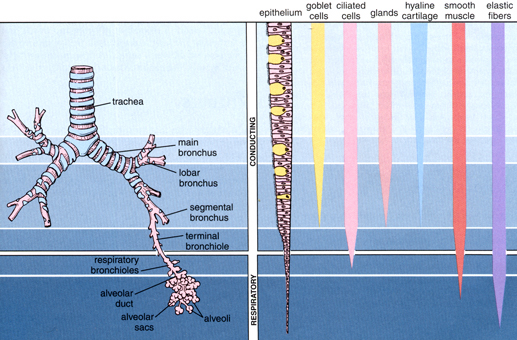
ANATOMY: Nose, Naso-pharynx, Pharynx, Trachea, Bronchi, Bronchioles (segmental and terminal), Respiratory bronchioles, Alveolar ducts Alveolar air sacs of infundibuli and Pulmonary alveoli are the anatomical components of respiratory system.
Nose: Each nasal cavity is lined with ciliated columnar epithelia and is highly vascular.
Larynx: Lined by ciliated columnar epithelia, except the true vocal cord, that is lined by stratified epithelia.
Trachea: 12 cm long and 15 mm diameter. Has series of C-shaped cartilages which is incomplete posteriorly. Inner most mucous membrane lined with ciliated columnar epithelia, covered with mucous. Goblet cells are seen in between the cilia. During inspiration trachea increases both in length and in diameter.
Bronchi: Resembles trachea, but cartilage forms a complete ring by pieces of cartilage which overlap each other and held together by connective tissues.
Lungs:
§ Alveoli communicate with each other through very minute vents.
§ Air and blood are separated in pulmonary alveoli by a very thin layer of flat alveolar cubical cells and pulmonary capillary endothelials.
§ Total pulmonary alveolar area of both lungs is about 80-90 m2.
§ Blood supply to lungs is by pulmonary arteries and its branches.
§ Additionally, bronchial arteries supply bronchial tubes, connective tissues and pleura.
§ Nerve supply through vagus (vasoconstrictor) and sympathetic (vasodilation).
Pleurae: Forms the outer covering of lungs. Consists of visceral and parietal layers lined by flat cubical cells and are separated from each other by a thin layer of pleural fluid.
 Normal
rate of respiration in adult: 16-18/min.
It is more in children. Increase in this rate is
also observed during hyperactivity, exercise, emotional states and high BMR.
Normal
rate of respiration in adult: 16-18/min.
It is more in children. Increase in this rate is
also observed during hyperactivity, exercise, emotional states and high BMR.
Alveoli: It is the primary site of gas exchange between air and blood. It is a very thin layer 0.1 - 1.5 µ allowing for rapid and efficient gas exchange. It has a rich capillary network that anastomoses through the wall of the alveoli, total endothelial surface area of about 125 m2 for gas exchange. The blood- air barrier consists of:-
F
Endothelial cell of capillary.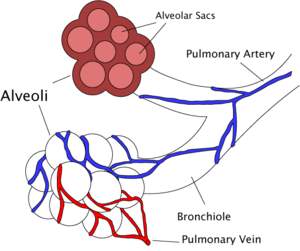
F Basement membrane between endothelial and epithelial cells.
F Epithelial cell (simple squamous) of alveolar lining.
F Surfactant layer.
§ The lungs contain about 3 x 108 alveoli, representing a total surface area of 70-90 m2, each wrapped in a fine mesh of capillaries.
§ The alveoli have radii of about 50 µm but increase to around 100 µm during inhalation.
§ The alveoli consist of an epithelial layer and extracellular matrix surrounded by capillaries. In some alveolar walls there are pores between alveoli.
§ There are 3 major alveolar cell types in the alveolar wall (pneumocytes):
§
Type I cells that form the
structure of an alveolar wall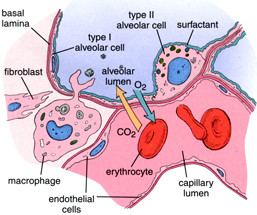
§ Type II cells that secrete surfactant to lower the surface tension of water and allow the membrane to separate thereby increasing the capability to exchange gases.
§ Type III cells are macrophages that destroy foreign material, such as bacteria.
§ The alveoli have an innate tendency to collapse (atelectasis) because of their spherical shape, small size, and surface tension due to water vapor. Phospholipids (surfactants) and the pores help to equalize pressures and prevent collapse.
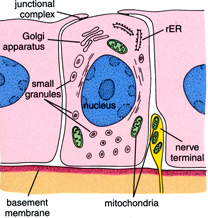
(Fig: Clara cells – secretes surfactants)
PULMONARY VOLUMES AND CAPACITIES
1. TIDAL VOLUME: Quantity of air taken in and given out at each normal quiet respiration. It is measured with spirometer. Normal value: 500 mL (0oC) and 600 mL (37oC).
2. COMPLEMENTAL OR INSPIRATORY RESERVE VOLUME: Amount of air taken in during forced inspiration over and above tidal volume. (1.5-2 L)
3. SUPPLEMENT OR EXPIRATORY RESERVE VOLUME: Amount of air given out during forced expiration after the end of quiet expiration. (1.3 L)
4. RESIDUAL VOLUME: Amount of air left behind in the lung at the end of forced expiration (1-1.4 L)
5. MINIMAL VOLUME: Amount of air which remains in the alveoli even after the collapse of lungs.
6. DEAD SPACE AIR: Air left in the bronchial tree, which does not take part in respiration (140 mL).
Total air X (Alveolar CO2 – Expired air CO2)
Dead space air = --------------------------------------------------------
% CO2 of alveolar air
7. RESPIRATORY (OR VENTILATION) MINUTE VOLUME: It is Respiration rate/min X Tidal volume. It rises even 10-fold during severe exercise
8. VITAL CAPACITY: The maximal amount of air given out by a subject after maximal deep inspiration. Measured with spirometer. It is thus, tidal air + complemental + supplemental air. Normal value: 3-3.3 L.
9. MAXIMAL BREATHING CAPACITY: Maximum amount of air ventilated by a person on breathing rapidly and deeply for 14 sec. Normal value: 100 L/min.
10. INSPIRATORY CAPACITY: Amount of air taken with maximum deep inspiration (2.5 L).
11. TOTAL LUNG CAPACITY: It is Vital capacity + Residual volume (5.5 L).
12. PULMONARY COMPLIANCE: The extensibility of lungs and thorax. It is represented by increase in volume in the lung for each unit increase in intra alveolar pressure. Normal value: 130 mL/cm H2O.
13. FUNCTIONAL RESIDUAL CAPACITY: Amount of air remaining in lungs after quiet expiration. It is thus, expiratory reserve volume + residual volume (2.5-3 L).
14. ALVEOLAR VENTILATION: (Tidal volume – dead space volume) X respiration rate/min (4.2-6.3 L/min).
15. ALVEOLAR AIR: The air that comes in direct contact with the pulmonary alveoli and takes part in gaseous exchange. (3 L/min or 2-2.5 L/m2 of body surface/min).
CHEMISTRY OF RESPIRATION
|
% |
Inspired air |
Expired air |
Difference |
|
O2 |
21% |
16% |
5% |
|
CO2 |
0.1% |
4.1% |
4% |
If the average respiration rate = 12/min
And tidal volume = 500 mL
Then, amount of inspired or expired air per min = 6000 mL/min
Thus, O2 consumed per min = (6000*5)/100 = 300 mL
And, CO2 given out per min = (6000*4)/100 = 240 mL
Therefore, Respiratory Quotient (RQ) which is the ratio of CO2 formed and O2 consumed simultaneously by a tissue = 240/300 = 0.8
PARTIAL PRESSURE OF GASES IN ALVEOLAR AIR
Total pressure of Alveolar air = 760 mmHg
Aqueous vapour pressure = 50 mmHg
Balance (pCO2 + pO2 + pN2) = 710 mmHg
Thus, pCO2 = (5.5*710)/100 = 39 mmHg
pO2 = (13.8*710)/100 = 98 mmHg
pN2 = (80.7*710)/100 = 573 mmHg
Factors which keep a gas in liquid are:
· Solubility Coefficient of the gas
· Partial Pressure (pressure exerted by an individual gas in a mixture of gases)
· Chemical Affinity
Henry’s Law: Concentration of dissolved gases in liquid = PP * solubility coefficient.
Normally from 100 mL of blood, 70 mL of gaseous mixture is obtained as follows:
|
GAS |
ARTERIAL BLOOD, mL % |
VENOUS BLOOD, mL % |
|
O2 |
19-20 |
12-13 |
|
CO2 |
50 |
56 |
|
N2 |
1-2 |
1-2 |
|
TOTAL |
70 |
70 |
ABSORPTION QUOTIENT is defined as “the amount of gas which is kept up by the fluid at n.t.p.” and is expressed in mL.
|
GAS |
PP, mmHg |
|||||
|
Inspired air |
Expired air |
Alveolar air (37oC) |
Art.blood |
Ven.blood |
Tissue |
|
|
O2 |
158.3 |
116 |
100 |
96 |
40 |
40 |
|
CO2 |
0.3 |
30 |
40 |
40 |
46 |
46-55 |
|
N2 |
596.4 |
575 |
568 |
547 |
570 |
- |
O2 CARRIAGE BY BLOOD
O2 is carried in blood in 2 forms, i.e., in (a) physical solution (0.3 mL %) and most of them in (b) with Hb as Oxy-Hb in loose combination. This combination takes stepwise:
Hb4 + O2 <---> Hb4O2
Hb4O2 + O2 <---> Hb4O4
Hb4O4 + O2 <-----> Hb4O6
Hb4O6 + O2 <-----> Hb4O8
This is the best example of positive cooperativity of a protein. 1 gm of Hb can carry 1.34 mL of O2.
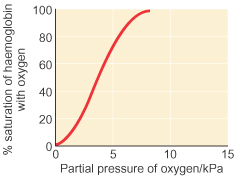
§ O2-nated blood from the lungs is supplied to tissues, where oxy-Hb is changed to reduced-Hb, which can be studied by O2 dissociation curve.
§ Total O2 capacity of blood = Oxy-Hb + O2 in physical solution (at 150 mmHg).
§ The O2 dissociation curve is plotted with O2 content of blood (or) Hb saturation % against O2 tension.
§ At 100 mmHg, Hb is 98% saturated (19 mL O2/dL blood).
§ Reduction of pressure causes release of O2 from Hb, so that, at 40 mmHg Hb is only 70% saturated (14 mL O2/dL blood).
§ Dissociation is complete at 0 mmHg, i.e., only reduced Hb is left.
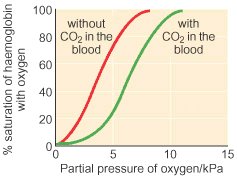
§ Increase in pCO2, [H+] and temperature causes increased dissociation of O2 from Hb, i.e., the curve shifts towards right. (graph)
§ Anemia lowers and polycythemia raises the curve.
§ The above said effect of pCO2 and H+ on O2 dissociation is known as Bohr’s effect.
§ Coefficient of O2 utilization = O2 taken by tissues/ O2 in arterial blood. This is usually 5/19*100 = 26%
§ Although blood is 95% saturated with O2 only 1/3rd is used for normal tissue supply. The remaining 2/3rd is reserved for emergency.
§ When O2 saturation decreases below 60%, signs of O2-deficiency develop.
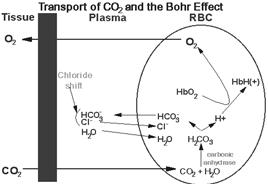
CO2 CARRIAGE BY BLOOD
CO2 is found in blood in 3 forms, viz., [a] Physical combination as H2CO3 (5%), [b] Chemical combination as HCO3 (65%), [c] Carbamino compound (30%).
Formation of this HCO3
In plasma: NaPr + H2CO3 <-----> HPr + NaHCO3 (Hb acting as buffer, where Pr- is proteinate which is Hb only).
Na2HPO4 + H2CO3 <-----> NaHCO3 + NaH2PO4 (phosphate buffer system)
In RBC,
H2CO3 + KHbO2 <-----> KHCO3 + HHb + O2
O2 + H2O <----------------------> H2CO3
Carbonic Anhydrase
 HAMBURGER
SHIFT or CHLORIDE SHIFT
HAMBURGER
SHIFT or CHLORIDE SHIFT
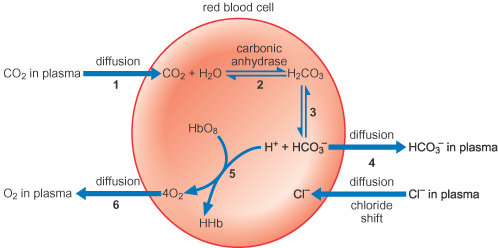
ü CO2 being permeable to RBC cell membrane, it enters the cells and reacts with KHb and forms KHCO3.
ü By this way more HCO3 is formed in RBCs than in plasma.
ü CA present in RBCs help to accelerate this reaction as said above.
ü This HCO3 formed in RBCs migrates out in to plasma, while K+ remains behind (impermeable).
ü Thus, RBCs become more positive inside.
ü To equilibrate the HCO3 loss, Cl- is transported in to the RBCs.
ü Thus, this high buffering capacity of RBCs overcomes the poor buffering of plasma.
[Cl-] cells/[Cl-] plasma = [HCO3-] cells/[HCO3-] plasma
ü Approximately 70% of HCO3- formed in RBCs migrates out to plasma due to this chloride shift.
|
|
ART.BLOOD |
VEN.BLOOD |
|
CO2 |
48 mL % |
52 mL % |
|
Plasma NaHCO3 |
38.1 % |
35.2 % |
|
RBC KHCO3 |
9.8 % |
10.5 % |
|
Carbamino Hb |
2 % |
2.6 % |
|
Carbamino plasma protein |
1 % |
1.1 % |
O2 causes CO2 dissociation shift towards right, i.e., it causes displacement of CO2 from Hb.
Carbamino compounds are formed in the RBCs in association with Hb, and in plasma with plasma proteins.
CO2 + Pr.NH2 <-----------------------> Pr.NH.COOH
This is not a stable compound and acts as mobile fraction of CO2.
BOHR’S EFFECT
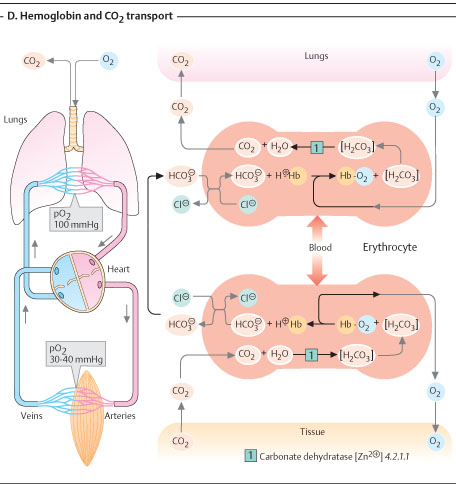
CARBONIC ANHYDRASE
M.wt. 30,000 Da. Contains Zn2+ as cofactor which is very essential for its activity.
It has 3 isoforms, viz., CA-A, CA-B and CA-C.
It is present in RBCs, Pancreas, Gastric mucosal membrane, Kidney and Brain.
Also present in minor amounts in red muscles, spleen, liver and salivary glands.
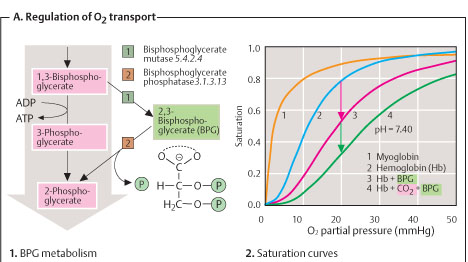
EFFECT OF 2, 3-DIPHOSPHOGLYCERATE ON O2 DISSOCIATION
1. RBCs have plenty of 2, 3-DPG molecules which are formed from 1, 3-DPG by the enzyme diphospho glycerate mutase.
2. This molecule is a highly charged anion that binds with β-chains of deO2-nated Hb.
3. It is not bound to that of O2-nated Hb.
HbO2 + 2, 3-DPG <------------> Hb-2, 3-DPG + O2
Thus, from the above reaction it is clear that ^ [2, 3-DPG] ----> ^ O2 dissociation.
Increased 2, 3-DPG levels are causes by androgens, thyroid hormones, growth hormones, muscular exercise and high altitude.
Decreased levels are caused by ^ [H+].
RESPIRATORY DISORDERS
The diseases which affect the physiology are:-
1. ACUTE RESPIRATORY DISTRESS SYNDROME (ARDS) is a severe inflammatory disease of the lung. Usually triggered by other pulmonary pathology, the uncontrolled inflammation leads to impaired gas exchange, alveolar flooding and/or collapse, and systemic inflammatory response syndrome. It usually requires mechanical ventilation in an intensive care unit setting.
2. INFANT RESPIRATORY DISTRESS SYNDROME (IRDS) is a syndrome caused by lack of surfactant in the lungs of premature infants.
3. In ASTHMA, the bronchioles, or the "bottle-necks" into the sac are restricted causing the amount of air flow into the lungs to be greatly reduced. It can be triggered by irritants in the air, photochemical smog for example, as well as substances that a person is allergic to.
4. EMPHYSEMA is another disease of the lungs, whereby the elastin in the walls of the alveoli is broken down by an imbalance between the production of neutrophil elastase (elevated by cigarette smoke) and alpha-1-antitrypsin (the activity varies due to genetics or reaction of a critical methionine residue with toxins including cigarette smoke). The resulting loss of elasticity in the lungs leads to prolonged times for exhalation, which occurs through passive recoil of the expanded lung. This leads to a smaller volume of gas exchanged per breath.
5. CHRONIC BRONCHITIS occurs when an abundance of mucus is produced by the lungs. The production of this substance occurs naturally when the lung tissue is exposed to irritants. In chronic bronchitis, the air passages into the alveoli, the broncholiotes, become clogged with mucus. This causes increased coughing in order to remove the mucus, and is often a result of extended periods of exposure to cigarette smoke.
6. CYSTIC FIBROSIS is a genetic condition caused by the dysfunction of a transmembrane protein responsible for the transport of chloride ions. This causes huge amounts of mucus to clog the bronchiolites, similar to chronic bronchitis. The result is a persistent cough and reduced lung capacity.
7. LUNG CANCER is a common form of cancer causing the uncontrolled growth of cells in the lung tissue. Due to the sensitivity of lung tissue, such malignant growth is often hard to treat effectively.
8. PNEUMONIA is an infection of the alveoli, which can be caused by both viruses and bacteria. Toxins and fluids are released from the virus causing the effective surface area of the lungs to be greatly reduced. If this happens to such a degree that the patient cannot draw enough oxygen from his environment, then the victim may need supplemental oxygen.
9. CAVITARY PNEUMONIA is a process in which the alveoli are destroyed and produce a cavity. As the alveoli are destroyed, the surface area for gas exchange to occur becomes reduced. Further changes in blood flow can lead to decline in lung function.
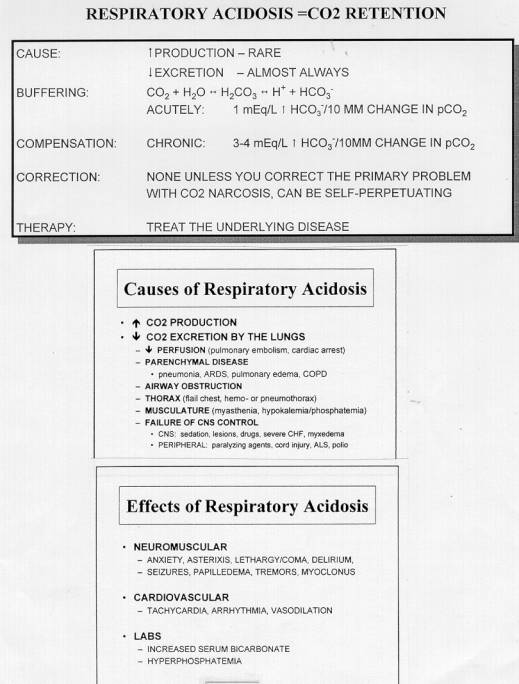
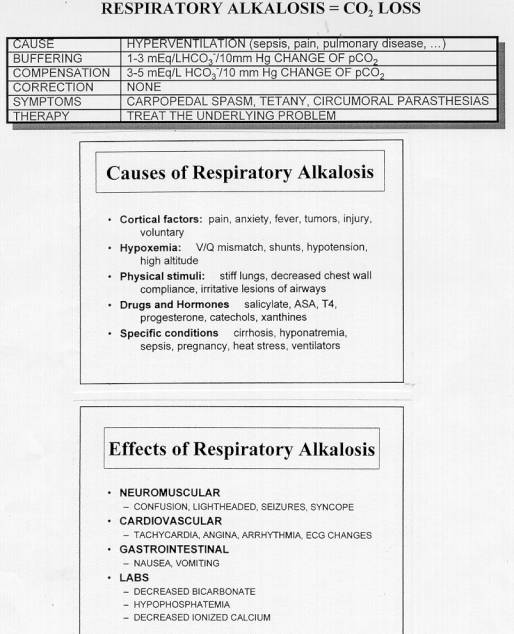
Respiratory acidosis and Respiratory alkalosis are the 2 major biochemical disturbances brought about by disorders of respiratory system. (See charts).